Dental aerosol management and infection control have come to the forefront of dentistry. As concerns over aerosol generating procedures and air filtration increase, the need for proper control methods is clear.
Sources are linked in blue throughout the article.
Use the sections below to quickly navigate to a specific area within this guide.
- Demand for a new standard of airborne infection control.
- Why Dental Air Filtration & Aerosol Management Are Needed
- Dental Aerosols and Infection Control Research
- A Complete List of Dental Infection Control Guidelines and Regulations for 2020
- Sources of Dental Aerosols and Airborne Contaminants in Dental Offices and Labs.
- 3 Ways to Effectively Capture Airborne Contaminants in Dental Offices and Labs.
- Where to Place Dental Air Filtration Equipment
- CDC Recommended Air Changes Per Hour for Dental Settings.
- Extraoral Suction Systems vs. High Volume Evacuators
- The Benefits of Better Air Quality
- Updates (As of July 2020)

Demand for a new standard of airborne infection control.
To be fair, there’s plenty of published material on dental aerosols, droplet transmission, and infection control however most of it’s not compiled or out dated.
Here’s an example of what I mean:
A 2004 JADA study, currently being referenced in many publications, stated that “The ADA has pointed out that it is unlikely that any dental treatment will be performed on a patient with active SARS…“
New research evidence for SARS-COV-2 suggests this is no longer the case.
One study published in Nature found that for every 100 cases of corona virus (a SARS variant) transmission, somewhere between 46 and 55 of them could be traced to a presymptomatic spreader with patients becoming infectious 2-3 days prior to showing symptoms. (see figure below)
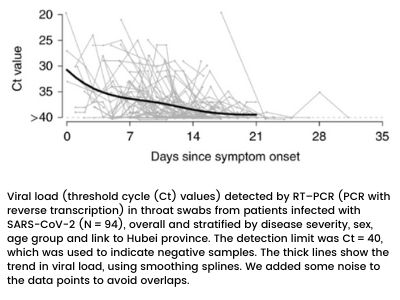
Despite the recent flip-flop from the World Health Organization, the CDC performed a comprehensive review of foreign and domestic data with multiple research studies ultimately publishing an online report titled, “Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic”.
The CDC report concluded that SARS-CoV-2 can be transmitted by persons with presymptomatic or asymptomatic infection.
Vaniman has been involved with dental air filtration for over 30 years. We’re not scientists, but we work with researchers, engineers, and clinicians to develop solutions for aerosol control and air filtration in the dental industry.
This article will focus on providing information and solutions using proven scientific data, recommended protocols, and a bit of plain ol’ common sense.
Why dental air filtration and aerosol management are needed.

Dental aerosols and other airborne hazards have ruthlessly affected dentists and their staff since the inception of dentistry nearly 9,000 years ago.
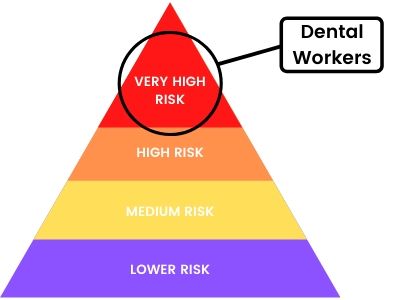
The hazard is so high that OSHA lists dental healthcare workers as a “very high risk” occupation for exposure to COVID-19.
This isn’t new information to most. Dentistry was always a dangerous professional long before the novel corona virus.
Bloodborne pathogens and percutaneous events have always been a risk. HBV, HCV and HIV in particular can infect dental workers as ADA studies have shown.
Luckily, these infection rates are quite low and there are plenty of safety protocols in place to minimize percutaneous infections.
Protection from aerosols and airborne contaminants are a different story.
The sad fact is that many dental professions didn’t consider air quality that big of a concern prior to COVID-19.
When looking at both older and newer research, it’s clear aerosols have been a primary cause of dental health issues.
Despite other recommendations common sense dictates that anytime you’re dealing with infectious blood or aerosols there is a risk of infection.
Dental Aerosols and Infection Control Research Up Till Now (2020)

From 1969-1971, two ground-breaking studies on dental aerosols were performed titled, “Studies on dental aerobiology. I. Bacterial aerosols generated during dental procedures” and “Studies on Dental Aerobiology: II. Microbial Splatter Discharged from the Oral Cavity of Dental Patients.”
These studies helped define “Aerosol” and “Splatter” in the dental field. (Aerosols are particles smaller than 50um while Splatter is anything larger)
The most profound finding in these studies was that aerosols are the greatest threat to infection in dentistry.
Over the years, researchers would further investigate dental aerosols.
A 1970 study named “Laminar Air Purge of Microorganisms in Dental Aerosols“, published in JADA, proved the benefits of using HEPA filtration to combat aerosols.
And in 2004, JADA published study called, “Aerosols and splatter in dentistry” that researched dental aerosols due to the advent of SARS and similar droplet-spread diseases–it also concluded that dental aerosols are a major infection threat to dentists, staff, and patients.
In 2010, “A pilot study of bioaerosol reduction using an air cleaning system during dental procedures” concluded that bioaerosols can be significantly reduced using an air cleaning system.
The 2013 study, “Risk of Contamination of Different Areas of Dentist’s Face During Dental Practices“, showed that the highest concentration of aerosolized contaminates on a dentist’s face was around the nose and inner eyes.
These studies, along with many others not mentioned here, were excellent additions to the field at the time however with the advent of SARS-COV-2, newer research suggests previous infection control procedures and air management should be reevaluated.
So, why is this important to dentists?
Infection control procedures, regulations, and guidelines are all based on how to protect against the threat and transmission of potential diseases.
Dentists may now have to operate under guidelines that treat every patient as a potential infection risk.
A recent 2020 study published in Science found that COVID-19 appears to be spreading through transmission of aerosols produced by asymptomatic people. Change citation format
A Complete List of Dental Infection Control Guidelines and Regulations for 2020
We dug through the most current recommendations and mandates to produce an abbreviated list of dental infection control guidelines below. Updated as of June 17, 2020.
1. Request that dental staff call patients prior to the scheduled appointment to ask questions about their current health status.
2.Advise patients to wear a face covering when entering the dental practice.
3. Limit the number of people who accompany a patient to the appointment. If possible, the patient should make the visit alone.
4. Assess all patients upon arrival; temperature checks may be completed.
5. Remove items such as toys or reading material in office waiting rooms, to limit potential transmission through high-touch surfaces.
6. Encourage social distancing practices by minimizing the number of patients in the waiting room by spacing appointments thoughtfully and perhaps by asking patients to wait in their car until the dental staff is ready to treat the patient.
7. Advise dental staff members to wear additional personal protective equipment (PPE) as appropriate, such as surgical masks or N95 masks, full face shields or goggles with side shields to ensure an environment that is as safe and healthy as possible for patients and the dental team.
8.Place hand sanitizer generously around the office for use, and ensure surfaces are cleaned regularly.
The CDC’s updated dental settings guidance offers additional recommendations such as how patients can be positioned in the dental chair during appointments and waiting 15 minutes before disinfecting patient treatment rooms after use for patients who may have or tested positive for COVID-19.
The ADA guidance also includes ways dentists and hygienists can reduce aerosols, such as the following:
9.Hand scaling when cleaning teeth rather than using ultrasonic scaling.
10. Use of high-velocity suction whenever possible.
11. Use of rubber dental dams whenever possible.
Below you’ll find the primary resources used to compile this data.
CDC Guidance for Dental Infection Control
Prior to the COVID-19 pandemic, the primary guidelines for dental office infection control and management were provided by the CDC in two formal documents:
- Guidelines for Infection Control in Dental Health-Care Settings — 2003
- Summary of Infection Prevention Practices in Dental Settings : Basic Expectations for Safe Care —2016
Once the pandemic began the CDC provided updated guidance here:
Additionally, the CDC recommends immunization guidelines for DHCP here:
ADA Guidance for Dental Infection Control
The current ADA guidance for dental infection control is basically to mirror the CDC’s recommendations. The ADA has resolved the following on their website titled, “Infection Control and Sterilization“.
Resolved, that it be ADA policy to support the implementation of standard precautions and infection control recommendations appropriate to the clinical setting, per the 2003 Guidelines for Infection Control in Dental Health Care Settings and the 2016 Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care from the Centers for Disease Control and Prevention (CDC),
and be it further
Resolved, that the ADA urges practicing dentists, dental auxiliaries and dental laboratories to keep up to date as scientific information leads to improvements in infection control,
and be it further
Resolved, that this policy includes implementation of CDC recommendations for vaccination and the prevention and management of exposures involving non-intact skin, mucous membranes and percutaneous injuries.
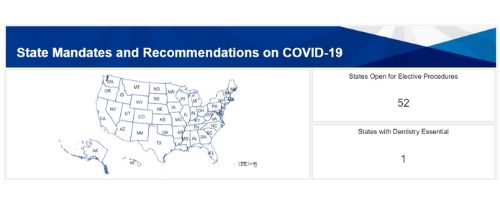
ADA Full List of State Specific Mandates
The ADA has produced an interactive map where you can select your specific state’s mandates.
OSHA Guidance for Dental Infection Control
OSHA has a slew of confusing regulations and standards which are listed here but we’ve reviewed the most pertinent ones for dentistry and listed them below.
OSHA’s Regulation on Bloodborne Pathogens
The scope of this regulation is for “all occupational exposure to blood or other potentially infectious materials”. Found here: 29 CFR 1910.1030
This applies mainly to saliva blood exposure during dental procedures more than airborne contaminants.
OSHA’s Regulation on Personal Protective Equipment
This applies the following PPE:
- Personal protective equipment for eyes, face, head, and extremities.
- Protective clothing
- Respiratory devices
- Protective shields and barriers
It basically states the the above PPE will be: “provided, used, and maintained in a sanitary and reliable condition wherever it is necessary by reason of hazards of processes or environment, chemical hazards, radiological hazards, or mechanical irritants encountered in a manner capable of causing injury or impairment in the function of any part of the body through absorption, inhalation or physical contact.“
OSHA’s Regulation on Respiratory Protection
This applies to anything involving “the control of those occupational diseases caused by breathing air”. Found here: CFR 1910.134
It focuses on PPE requirements and air management engineering controls which we will detail further in this article.
List of State Specific OSHA State Plans for Infection Control
Similarly to the ADA, OSHA has also produced an interactive state specific map for standards.
A full up to date list of state specific OSHA regulations can be found here: OSHA State Plans
While dental infection control recommendations and guidelines address precautions they do not address the primary sources.
Sources of airborne contaminants in dental offices and labs.
Airborne hazards in dental labs and offices can be classified as either biological or chemical.
Aerosols are particles less than 50 micron in diameter which are naked to the human eye.
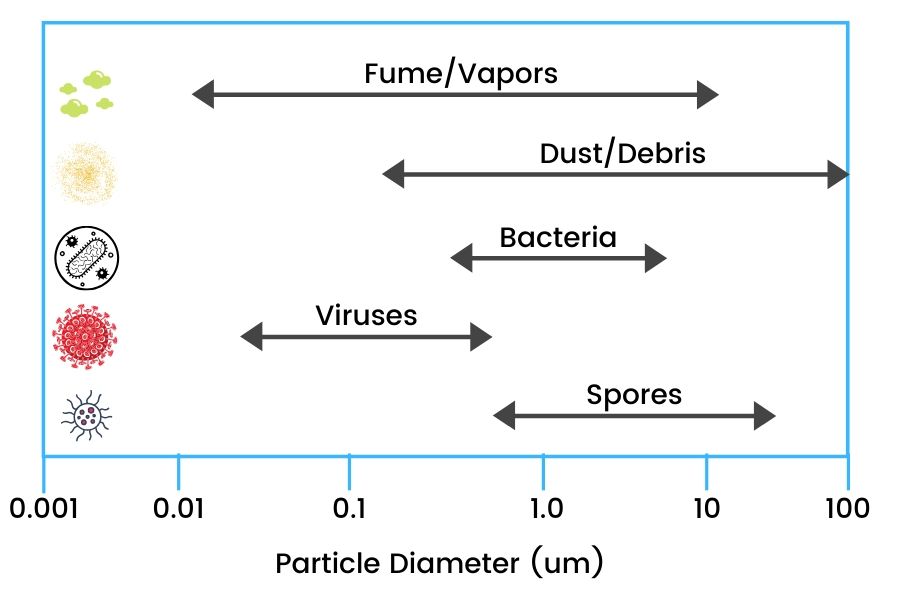
The smaller particles of an aerosol (0.5 to 10 μm in diameter) or droplet have the potential to penetrate and lodge in the smaller passages of the lungs and are thought to carry the greatest potential for transmitting infections.
Biological Aerosols
Biological aerosols come from patients and staff inside the dental office or lab so it’s helpful to identify the primary generating sources for proper infection control.
Patients and staff who are symptomatic or presymtopmatic emit biological aerosols through coughing, sneezing, and contaminating surfaces through touch.
It’s important to note that Biological particles usually become airborne from liquid or powder forms, so these particles are usually larger than ~0.5 um.
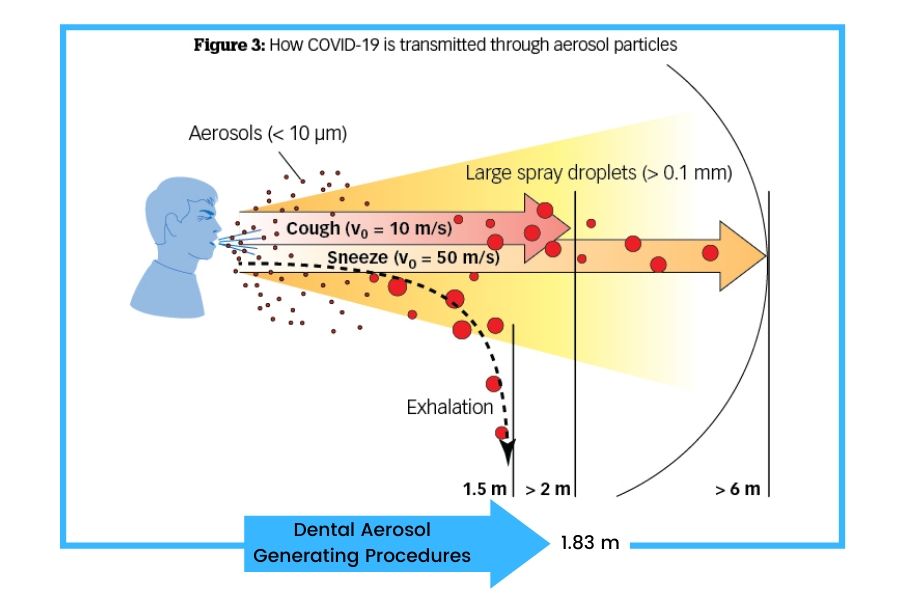
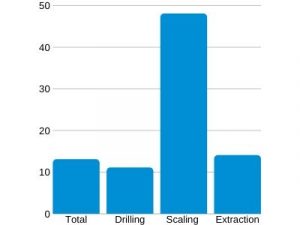
Dental aerosols produced from dental procedures like scaling produce the highest amount of aerosols for droplet transmission.
Aerosols have been reported to remain in the air anywhere from 30 minutes to 3 hours.
In summary, biological contaminants come from the following:
- Ambient Air
- Created from: Sneezing, Coughing, Particle Hang
- Located: Waiting Areas, Break Rooms, Bathrooms, Etc
- Aerosol Generating Procedures
- Created from: Scaling, Polishing, Grinding
- Located: Operatory, Lab, Spreads if Not Captured
- Surfaces Where Particles Fall or Touch
- Created from: Touches Surfaces, Particle Fall
- Located: Waiting Areas, Break Rooms, Bathrooms, Etc
Chemical Aerosols
Chemical aerosols and hazards present an ongoing threat to dental professionals and have been linked to several respiratory diseases.
Below is a list of none chemical hazards found in dental offices and labs.
Silica
Crystalline silica is found in alginate impressions, dental porcelains, and dental models or casts.
According to an OSHA fact sheet published in 2013, more than 41,000 workers in dental laboratories were exposed to respirable crystalline silica.
Metal
Metals found in amalgams and crowns can be extremely dangerous.
Mercury vapor can be released during procedures and can affect patients and staff.
Waste Anesthetic Gases
Waste anesthetic gases are common in dentistry and are emitted from system leaks or patient exhaled breath.
One of the challenges of managing WAG exposure is the lack of detectable odor until very high concentrations are reached which affect the judgement of staff to recognize the leak.
Sterilants and Disinfectants
Now that more offices and labs are implementing infection control procedures, harmful exposure to chemical disinfectants and sterilants may become a risk.
Some studies have shown that prolonged exposure can cause mucous membrane and respiratory health effects.
Risks of mucous membrane irritation and asthma in health care workers should be considered in development of disinfection protocols.
Lasers
Lasers present an airborne threat through the inhalation of vapor or surgical smoke.
It should be noted that the level of training and experience dental staff receive is generally far less than the typical laser surgical nurse or hospital laser safety officer.
Waterborne Bacteria
Several procedures in dentistry may result in the aerosolization of building water.
Legionella, Pseudomonas, and Mycobacterium species can colonize domestic water systems.
Often, the dental office or clinic does not have the responsibility or authority to manage and the building’s domestic water systems.
You can find revised guidelines for building water from ASHRAE here.
Chemical sources aren’t generated unless someone interacts with them.
For example, mercury vapor from amalgam isn’t a concern unless you’re grinding on it.
Remember to be mindful of using chemicals in general as prolonged exposure can have consequences.
How to effectively capture airborne contaminants in dental offices and labs.
After reviewing countless recommendations and guidelines paired with Vaniman’s 30 years of experience we’ve found that there are three primary methods for dental aerosol management in order to maintain good air quality.
1. Source Control

Source control involves limiting airborne contaminants at their source.
Methods of source control.
- FDA Approved Face Masks
- Medical Face Shields
- Surface Disinfection Procedures
- Eye Protection
- Physical Barriers & Guards
The goal of source control is to lower airborne transmission of aerosols. This is only part of the solution as there is still a high potential for infection if used alone.
Source Control Pros & Cons
Pros:
- Relatively inexpensive.
- Minor disruption to existing workflow.
Cons:
- Fails to fully protect patients and staff.
- Does not remove contaminants from air.
2. Source Capture

Source capture grabs the aerosols and contaminants and prevents them from re-entering the air.
This is extremely effective when used with dental aerosol generating procedures.
Methods of source capture.
- Extraoral Suction Systems
- High Volume Evacuators (HVE)
These systems are extremely effective at capturing aerosols generated during dental procedures.
Source Capture Pros & Cons
Pros:
- Captures invisible particles generating during dental procedures.
- Gives patients/staff good perception of safety.
- Removes contaminants from air.
Cons:
- Requires equipment purchase.
- May require modification to existing lines and equipment.
- Moderately disruptive during procedures.
View our section below for a comparison between extraoral and intraoral suction systems.
3. Air Exchange

Using air exchange as a method of air quality and control continuously cycles and filters the air free from chemical and biological particulates.
Methods of air exchange and filtering.
These systems filter the air through the use of special filter mechanisms or disinfection through UV light.
HVAC Systems in Dental Settings
HVAC systems use a combination of HEPA or UVGI mechanisms to capture or eradicate contaminants.
It should be noted that HVAC system design is key for proper filtration to occur. The physics behind how HEPA filters and UV light works requires specific exposure and air flow rates to work properly.
Because of these factors, HVAC systems are not a feasible option in most dental settings.
HVAC Systems Pros & Cons
Pros:
- Air throughout building can be continuously cycled and filtered at optimal air flow rates.
Cons:
- Requires special design considerations for air flow and ducting.
- High maintenance costs to access ducting and make repairs.
UVGI Use in Dental Settings

UV light is generally dangerous to humans. Not to mention bulbs used to produce UV light can emit Ozone; a dangerous byproduct.
Typically, UVGI is used in hospitals however with the rise of SARS related diseases these systems are gaining more interest.
Caution should be used when exploring UVGI methods. As of June 2020, the CDC currently only recommends the use of UV light for disinfection in specially designed HVAC systems or special light fixtures.
UVGI requires a very specific amount of time and exposure for it to properly irradiate and destroy viruses.
To date, no scientific research has been presented validating its effectiveness inside portable filtration or extraoral suction devices.
In fact, a recent study showed UV light inside these devices to be “inconclusive” and concluded the following:
“Given the uncertainty of the estimate of benefits, an in-room air cleaner with HEPA technology only may be an equally reasonable alternative to using one with combined UVGI and HEPA technology. This is primary due to the requirements for UV light to work; mainly exposure time and light intensity”
Air Cleaning Technologies: An Evidence-Based Analysis
Ont Health Technol Assess Ser. 2005; 5(17): 1–52.
This is due to the nature of air filtration systems which quickly move high amounts of air without giving the UV light adequate time to disintegrate more durable pathogens.
Manufacturers of such products should supply 3rd party research which validates any claims regarding UVGI efficacy.
For more on UV light inside HEPA filtration devices see our article titled, “Does UV Light Destroy Viruses in HEPA Filtration Devices?“
UVGI System Pros & Cons
Pros:
- Can efficiently eradicate biological hazards in affected air flow.
Cons:
- Requires special design considerations for air flow and exposure.
- Potentially hazards from UV bulbs and light exposure.
HEPA air filtration in dental settings.
To verify the efficacy of HEPA filtration devices, a study published in Dental Economics was performed on air quality pre and post air filtration.
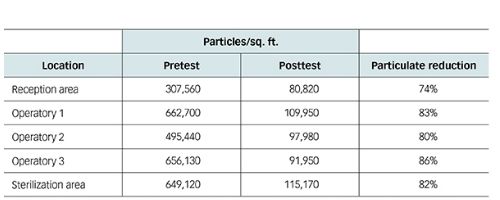
The results are blatantly obvious. While nothing is perfect, combining multiple capture and control methods will significantly cut down aerosol exposure.
If you’re still a skeptic on the capture potential of HEPA air purifiers you can learn more in our recent article titled, “Do HEPA air purifiers filter out the COVID-19 virus?“
Multiple studies lend credence to the benefits of air filtration and recommend the use of medical-grade air purifiers.
- Journal of Dental Hygiene
- Jacks ME. A laboratory comparison of evacuation devices on aerosol reduction. J Dent Hyg. 2002;76(3):202-206.
- International Journal of Dentistry
- Leggat PA, Kedjarune U. Bacterial aerosols in the dental clinic: a review. Int Dent J. 2001;51(1):39-44.
- Journal of the American Dental Association
- Godwin CC, Batterman SA, Sahni SP, Peng CY. Indoor environment quality in dental clinics: potential concerns from particulate matter. Am J Dent. 2003 Aug;16(4):260-266.
- British Dental Journal
- Hallier C, Williams DW, Potts AJ, Lewis MA. A pilot study of bioaerosol reduction using an air cleaning system during dental procedures. Br Dent J. 2010;209(8):E14.
- University of Athens
- Helmis GC, Tzoutzas J, Flocas HA, et al. Indoor air quality in a dentistry clinic. Sci Total Environ. 2007;377(2-3):349-365.
- SRM Journal of Research in Sciences Dental
- Yadav N, Agarwal B, Maheshwari C. Role of high-efficiency particulate arrestor filters in control of air borne infections in dental clinics. J Res Med Sci. 2015;6(4):240-242.
- Tsinghua University Bejing
- Chen C, Zhao B, Cui W, Dong L, An N, Ouyang X. The effectiveness of an air cleaner in controlling droplet/aerosol particle dispersion emitted from a patient’s mouth in the indoor environment of dental clinics. J R Soc Interface. 2010;7(48):1105-1118.
Studies compiled thanks to Dental Economics.
Where to place dental air filtration equipment.

Placement of air filtration equipment is key for optimal operation in dental offices and labs.
For dental offices, operatories and patient areas where the majority of aerosols are created are idea for air filtration equipment.

Placement of upward facing exhaust filtration systems underneath HVAC intake vents help push filtrated air throughout the entire office.
For dental labs, place filtration units in rooms where the aerosol created from grinding and polishing is highest, or use in milling rooms to lower fumes.
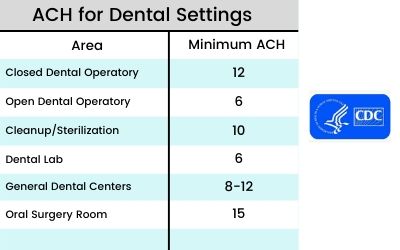
CDC recommended air changes per hour for dental settings.
The CDC has produced a chart providing recommended air changes per hour (ACH) based on the dental setting.
Air change rates are used to set an ideal estimate for efficient contaminant removal.
This is a key concept when using air filtration equipment as the ambient air must be cycled through the filtration system several times to ensure the area has been cleaned.
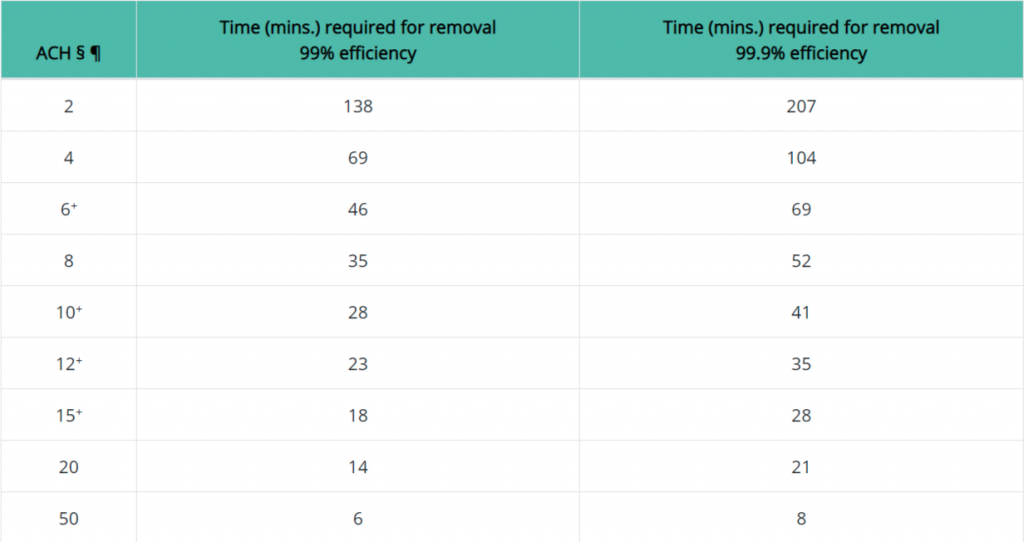
Below is a more definitive removal chart which correlates contaminant removal efficiency.
This chart is more accurate as it’s based on air changes rather than a general dental setting.
As you can see, higher ACH rates result in more efficient air filtration.
What is ACH or ACPH?
ACH or ACPH stands for Air Changes per Hour and is commonly referred to as “air exchange rate” or “air change rate”. It is a measurement of how many times a volume of air within a room will be added, removed, or exchanged with filtered clean air.
How do you calculate ACH or Air Changes per Hour?
To calculate Air Changes Per Hour (ACH), find the CFM of your device and multiply that by 60 then divide that total by the total cubic square feet of the room to get your total ACH.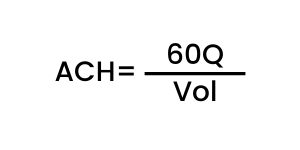
Q= CFM of filtration device
Vol= Room Volume
ACH Calculator Tool
If you’re in need of a calculation tool for Air Changes Per Hour click the button below.
Settle Time Calculator
What is settle time?
The “settle time” is the amount of time needed to remove infectious airborne organisms from room air or infectious aerosols that may be created during an AGMP.
This begins when the source of infectious aerosols ends.
Examples:
- When a patient on continuous Airborne Precautions is moved out of the room.
- Following an AGMP when a pathogen or virus (e.g., COVID-19) has the potential to be aerosolized during the procedure.
The “settle time” is used to guide if a N95 respirator needs to be worn while in the room or how long the room must sit before Housekeeping can begin cleaning.
The “settle time” should never impact patient care needs and should not delay essential patient or staff movement in and out of the room.
How is the room “settle time” determined?
To determine a specific “settle time” for a specific room, the number of Air Changes per Hour (ACH) must be evaluated as each room can be different (size, temperature, humidity, ventilation capacity, etc.).
The higher the ACH, the less time is required for settle time.
If the number of ACH for the patient room is known, a specific “settle time” can be calculated using the tool below.
Calculators based on CDC recommendations and formulas found here.
Extraoral Suction Systems vs. High Volume Evacuators

In regards to capturing aerosols generated during dental procedures many are turning to the use of extraoral suction systems and high volume evaculators (HVEs).
We’ll help compare the use of each system by listing pros and cons for each.
Extraoral Suction Systems
Pros:
- Hands free operation.
- Easier to maintain.
- No modifications or additional suction lines needed.
- Captures aerosols and ambient air which protects both patient and staff.
- Provides room air changes while in operation.
Cons:
- Equipment takes up space near chair.
- May require adjustment for various approaches.
- Some units can be extremely loud. (Vaniman units are only 53dB some go as high as 70dB)
High Volume Evacuators (HVE)
Pros:
- Uses little space.
- Excellent intraoral aerosol capture protecting staff.
- Many offices already using prior to pandemic.
Cons:
- Does not capture nasal aerosols or breathing from patient.
- May require additional compressor lines.
- Some patients have issues with HVE system in mouth (elderly, children).
- May require use of hand to hold. Newer systems are hands free.
The benefits of better air quality.

Dental offices using source control, source capture, and air exchange can drastically improve air quality and lower chances of infection.
The added benefit to proper air management and aerosol capture result in long term health benefits through lowering exposure to airborne hazards.


Please feel free to comment with any suggestions regarding this article. We openly welcome feedback from our readers.